2022年,美国泌尿外科学会(AUA)发布了最新的临床局限性前列腺癌指南,上次发表还是2018年。我们翻译整理了指南的建议汇总,内容包括风险评估、分期、基于风险的管理、管理原则和治疗后随访。供各位学习交流。
Clinically Localized Prostate Cancer: AUA/ASTRO Guideline (2022)
临床局限性前列腺癌:AUA/ASTRO指南(2022)
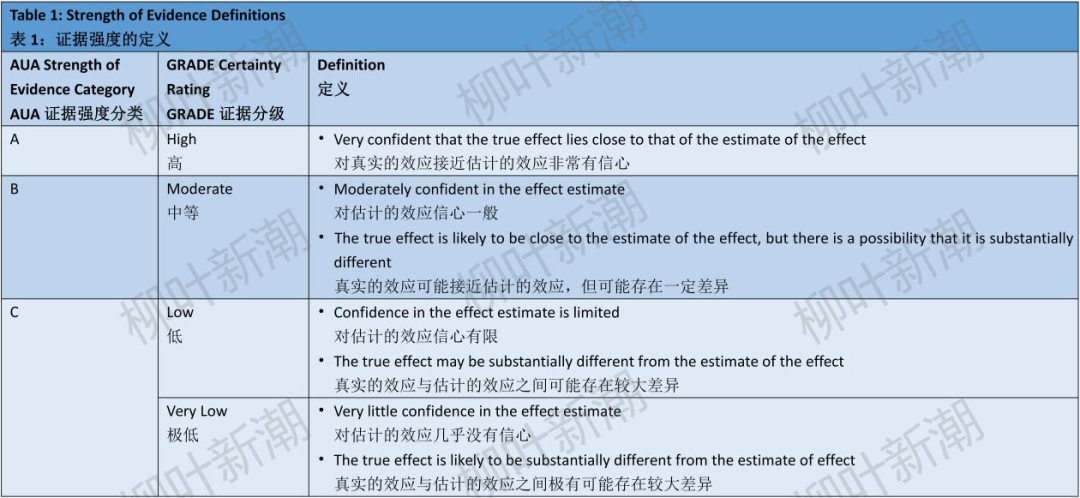
The recommendations discussed herein for the management of clinically localized prostate cancer provide a framework stratified by risk to facilitate care decisions and guide clinicians in the implementation of selected management options.
本文讨论了临床局限性前列腺癌的管理建议,提供了一个按风险分层的框架,以促进管理决策,并指导临床医生实施选定的管理方案。
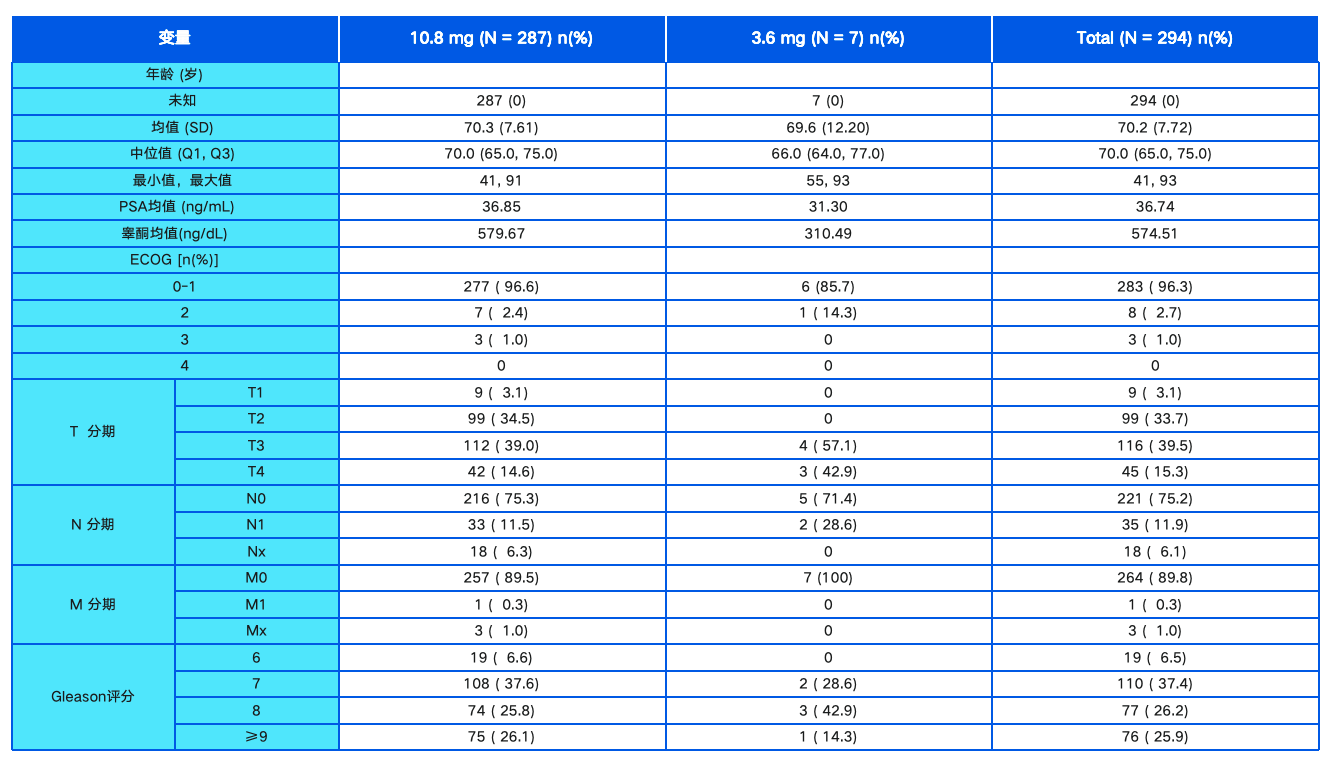
The systematic review that informs this Guidelines was based on searches in Ovid MEDLINE (September 2021), Cochrane Central Register of Controlled Trials (August 2021), and Cochrane Database of Systematic Reviews (September 2021). Searches were supplemented by reviewing reference lists of relevant articles. Criteria for inclusion and exclusion of studies were based on the Key Questions and the populations, interventions, comparators, outcomes, timing, types of studies and settings (PICOTS) of interest. The target population was patients with clinically localized prostate cancer, defined as up to clinical stage T3 (by digital rectal examination [DRE]) prostate cancer without nodal or distant metastasis (N0M0) on conventional imaging.
为了为本指南提供依据,检索Ovid MEDLINE(2021年9月)、Cochrane Central Register of Controlled Trials(2021年8月)和Cochrane Database of Systematic Reviews(2021年9月),进行系统性回顾。查阅相关文章的参考文献,进行补充。研究的纳入和排除标准基于关键问题以及PICOTS框架(人群、干预、对照、结局、时间、研究类型和场景)。目标人群是临床局限性前列腺癌患者,定义为≤临床T3期(通过直肠指检[DRE])前列腺癌,且常规影像学检查没有发现淋巴结或远处转移(N0M0)。



Risk Assessment
风险评估
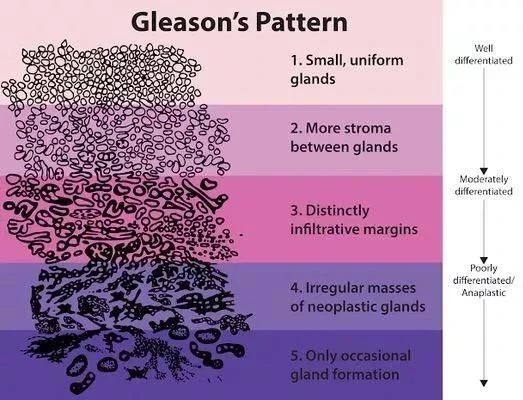
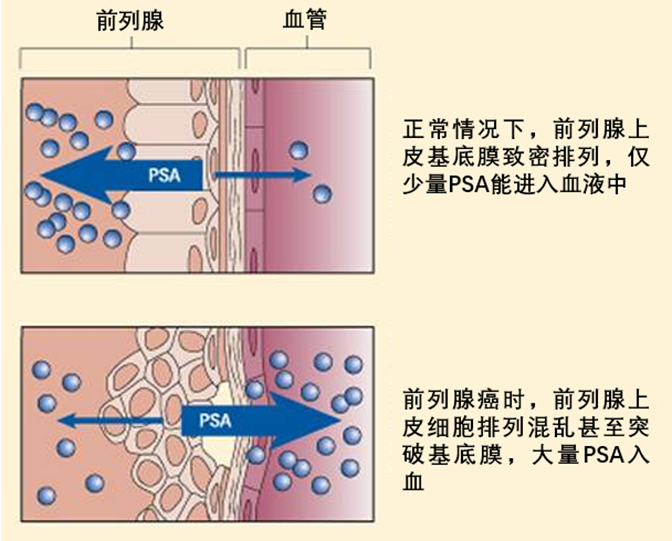
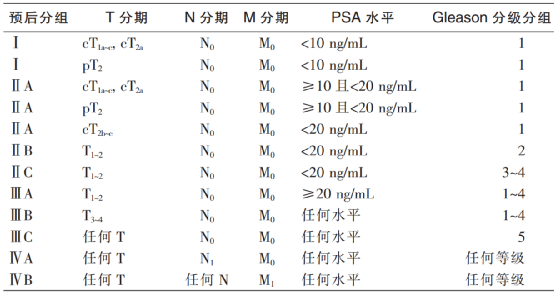
1. Clinicians should use clinical T stage, serum prostate-specific antigen (PSA), Grade Group (Gleason score), and tumor volume on biopsy to risk stratify patients with newly diagnosed prostate cancer. (Strong Recommendation; Evidence Level: Grade A)
临床医生应使用临床T期、血清前列腺特异性抗原(PSA)、分级分组(格里森评分)和活检组织中肿瘤所占体积来对新诊断的前列腺癌患者进行风险分层。(强烈推荐;证据水平:A级)
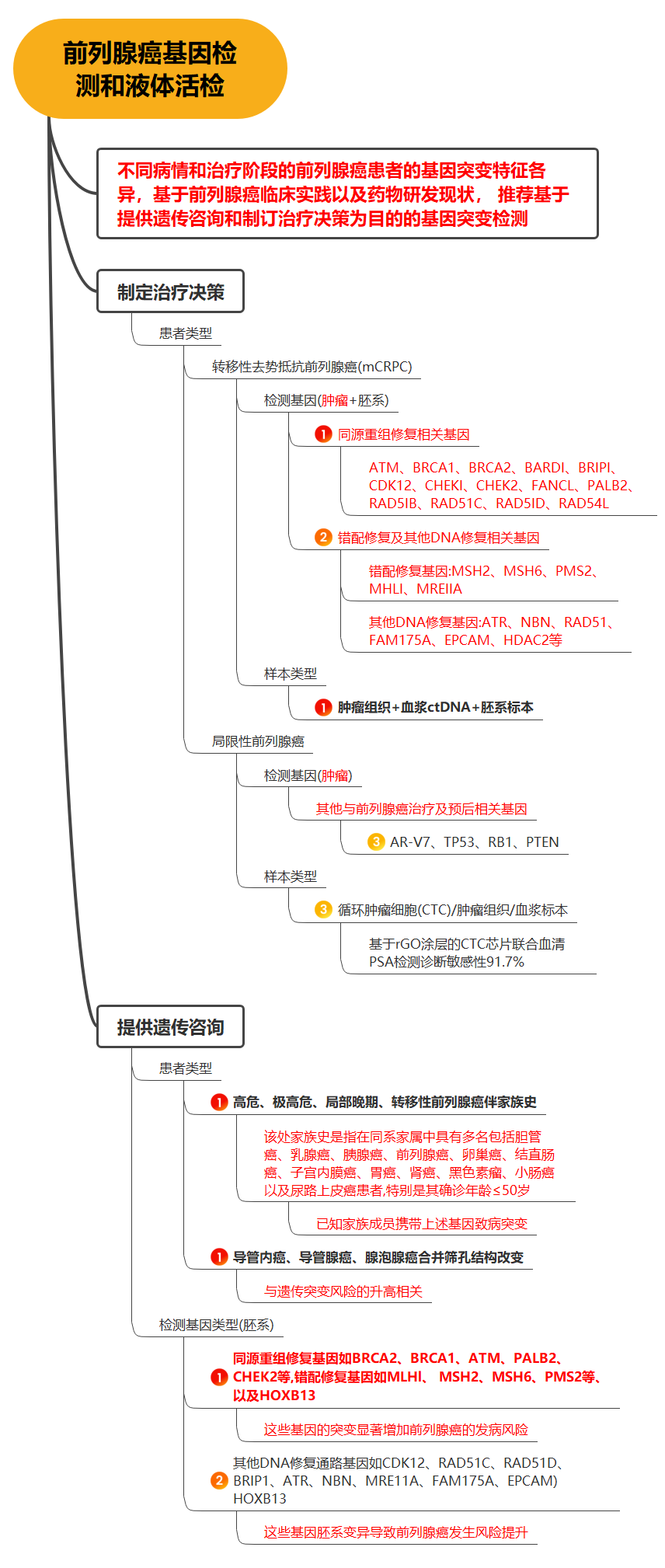
2. Clinicians may selectively use tissue-based genomic biomarkers when added risk stratification may alter clinical decision-making. (Expert Opinion)
当进行风险分层可能改变临床决策时,临床医生可以选择性使用基于组织的基因组生物标志物。(专家意见)
3. Clinicians should not routinely use tissue-based genomic biomarkers for risk stratification or clinical decision-making. (Moderate Recommendation; Evidence Level: Grade B)
临床医生不应常规使用基于组织的基因组生物标志物进行风险分层或临床决策。(中等推荐;证据水平:B级)
4. Clinicians should perform an assessment of patient and tumor risk factors to guide the decision to offer germline testing that includes mutations known to be associated with aggressive prostate cancer and/or known to have implications for treatment. (Expert Opinion)
临床医生应该对患者和肿瘤风险因素进行评估,以指导是否进行种系基因检测,包括评估是否具有与侵袭性前列腺癌相关的突变和/或对治疗有影响的突变。(专家意见)
Staging
分期
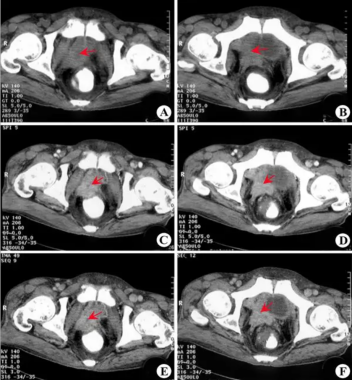
5. Clinicians should not routinely perform abdomino-pelvic computed tomography (CT) scan or bone scan in asymptomatic patients with low- or intermediate-risk prostate cancer. (Expert Opinion)
对于无症状的低危或中危前列腺癌患者,临床医生不应常规进行腹部-盆腔计算机断层扫描(CT)或骨扫描。(专家意见)
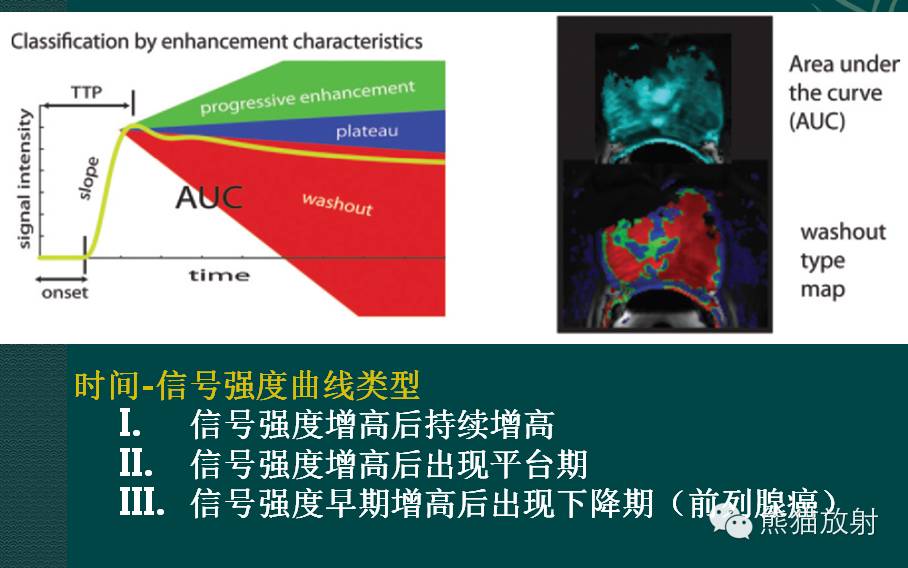
6. Clinicians should obtain a bone scan and either pelvic multi-parametric magnetic resonance imaging (mpMRI) or CT scan for patients with high-risk prostate cancer. (Strong Recommendation; Evidence Level: Grade B)
对于高危前列腺癌患者,临床医生应进行骨扫描和盆腔多参数磁共振成像(mpMRI)或CT。(强烈推荐;证据水平:B级)
7. In patients with prostate cancer at high risk for metastatic disease with negative conventional imaging, clinicians may obtain molecular imaging to evaluate for metastases. (Expert Opinion)
对于常规影像学检查为阴性但转移风险较高的前列腺癌患者,临床医生可进行分子影像学检查,以评估转移情况。(专家意见)
Risk-Based Management
基于风险的管理
8. Clinicians should inform patients that all prostate cancer treatments carry risk. The risks of treatment, in particular to patients' urinary, sexual, and bowel function, must be incorporated with the risk posed by the cancer, patient life expectancy, comorbidities, pre-existing medical conditions, and patient preferences to facilitate a shared decision-making approach to management. (Clinical Principle)
临床医生应告知患者,所有的前列腺癌治疗都有风险。必须要将治疗的风险,特别是对患者的泌尿功能、性功能和肠道功能造成的风险,与癌症造成的风险、患者的预期寿命、合并症、已有的其他疾病和患者偏好一同考虑在内,从而共同决定患者的管理方法。(临床原则)
9. Clinicians should provide an individualized risk estimate of post-treatment prostate cancer recurrence to patients with prostate cancer. (Clinical Principle)
临床医生应对前列腺癌患者进行治疗后前列腺癌复发的个性化风险评估。(临床原则)
10. For patients with low-risk prostate cancer, clinicians should recommend active surveillance as the preferred management option. (Strong Recommendation; Evidence Level: Grade A)
对于低危前列腺癌患者,临床医生应推荐主动监测作为首选的管理方案。(强烈推荐;证据水平:A级)
11. In asymptomatic patients with prostate cancer and limited life expectancy (determined on a patient-specific basis), clinicians should recommend watchful waiting. (Strong Recommendation; Evidence Level: Grade A)
对于无症状和预期寿命有限(根据患者具体情况确定)的前列腺癌患者,临床医生应推荐观察等待。(强烈推荐;证据水平:A级)
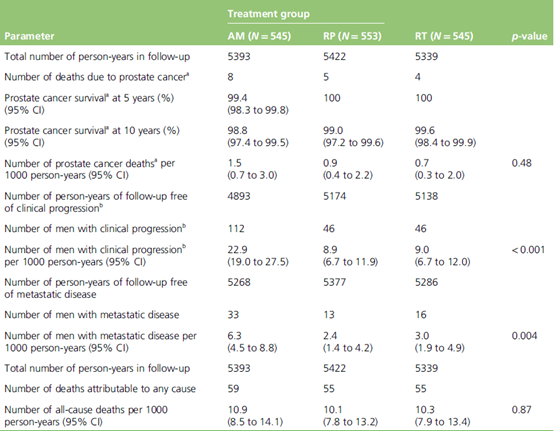
12. For patients with favorable intermediate-risk prostate cancer, clinicians should discuss active surveillance, radiation therapy, and radical prostatectomy. (Strong Recommendation; Evidence Level: Grade A)
对于具有良好特征的中危前列腺癌患者,临床医生应讨论主动监测、放疗和根治性前列腺切除术。(强烈推荐;证据水平:A级)
13. Clinicians should inform patients with intermediate-risk prostate cancer considering whole gland or focal ablation that there are a lack of high-quality data comparing ablation outcomes to radiation therapy, surgery, and active surveillance. (Expert Opinion)
临床医生应告知考虑全腺体消融或局灶消融的中危前列腺癌患者,目前缺乏比较消融治疗与放疗、外科手术和主动监测治疗结局的高质量数据。(专家意见)
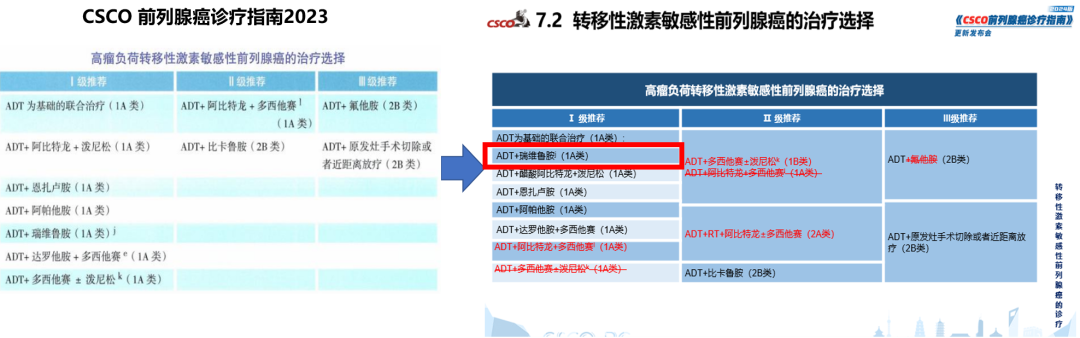
14. For patients with unfavorable intermediate- or high-risk prostate cancer and estimated life expectancy greater than 10 years, clinicians should offer a choice between radical prostatectomy or radiation therapy plus androgen deprivation therapy (ADT). (Strong Recommendation; Evidence Level: Grade A)
对于高危或具有不良特征的中危前列腺癌患者,如果预期寿命超过10年,临床医生应提供根治性前列腺切除术或放疗+雄激素剥夺疗法(ADT)两种选择。(强烈推荐;证据水平:A级)
15. Clinicians should not recommend whole gland or focal ablation for patients with high-risk prostate cancer outside of a clinical trial. (Expert Opinion)
临床医生不应推荐在临床试验之外对高危前列腺癌患者进行全腺体消融或局灶消融。(专家意见)
16. Clinicians may recommend palliative ADT alone for patients with high-risk prostate cancer, local symptoms, and limited life expectancy. (Expert Opinion)
对于有局部症状且预期寿命有限的高危前列腺癌患者,临床医生可建议单纯姑息性ADT。(专家意见)
PRINCIPLES OF ACTIVE SURVEILLANCE
主动监测的原则
17. Patients managed with active surveillance should be monitored with serial PSA values and repeat prostate biopsy. (Expert Opinion)
对于选择主动监测的患者,应通过连续的PSA值和重复前列腺活检进行监测。(专家意见)
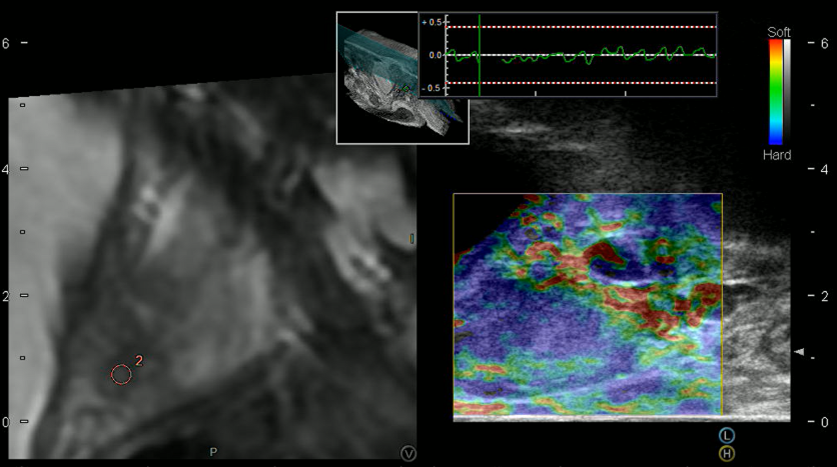
18. In patients selecting active surveillance, clinicians should utilize mpMRI to augment risk stratification, but this should not replace periodic surveillance biopsy. (Expert Opinion)
对于选择主动监测的患者,临床医生应利用mpMRI来改善风险分层,但这不应该取代定期监测活检。(专家意见)
PRINCIPLES OF SURGERY
外科手术的原则
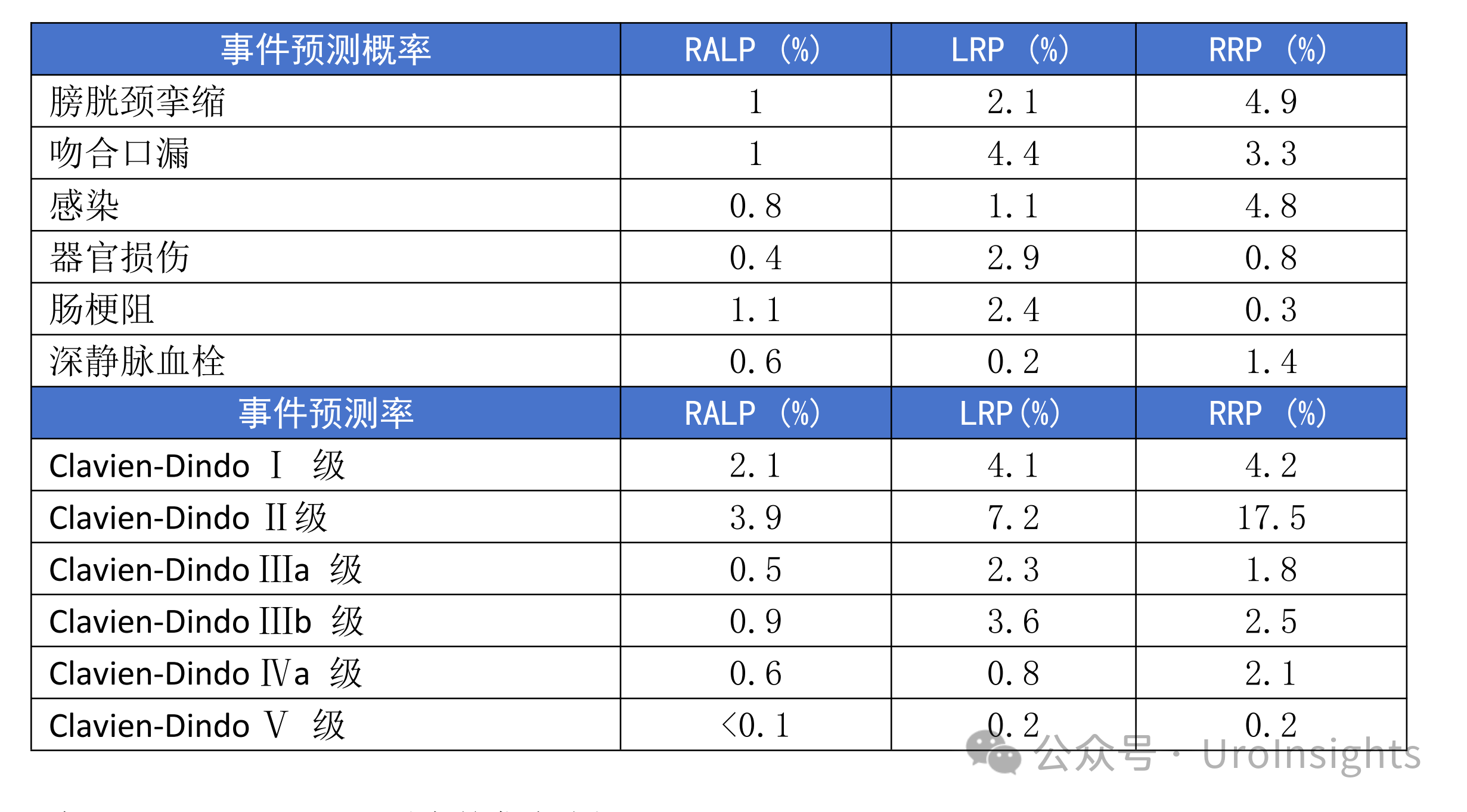
19. In patients electing radical prostatectomy, nerve-sparing, when oncologically appropriate, should be performed. (Moderate Recommendation; Evidence Level: Grade B)
对于选择根治性前列腺切除术的患者,在肿瘤情况合适的情况下,应进行保留神经的手术。(中等推荐;证据水平:B级)
20. Clinicians should inform patients that pelvic lymphadenectomy provides staging information, which may guide future management, but does not have consistently documented improvement in metastasis-free, cancer-specific, or overall survival. (Moderate Recommendation; Evidence Level: Grade B)
临床医生应告知患者,盆腔淋巴结切除术可提供分期信息,可以指导未来的管理,但目前尚无一致数据说明其可改善无转移生存、癌症特异性生存或总生存。(中等推荐;证据水平:B级)
21. Clinicians should use nomograms to select patients for lymphadenectomy. The potential benefit of identifying lymph node positive disease should be balanced with the risk of complications. (Clinical Principle)
临床医生应使用诺模图来选择适合淋巴结清扫术的患者。识别阳性淋巴结有潜在益处,但也要注意可能出现并发症,需要在这两者之间进行平衡。(临床原则)
22. Clinicians performing pelvic lymphadenectomy should perform an extended dissection, which improves staging accuracy compared to a limited dissection. (Moderate Recommendation; Evidence Level: Grade: B)
临床医生在进行盆腔淋巴结清扫术时,应扩大清扫范围,与局限性淋巴结清扫术相比,扩大的淋巴结清扫术可提高分期评估的准确性。(中等推荐;证据水平:B级)
23. Clinicians should complete a radical prostatectomy if suspicious regional nodes are encountered intraoperatively. (Moderate Recommendation; Evidence Level: Grade C)
如果在术中遇到可疑的区域性淋巴结,临床医生应继续完成根治性前列腺切除术。(中等推荐;证据水平:C级)
24. Clinicians should risk stratify patients with positive lymph nodes identified at radical prostatectomy based on pathologic variables and postoperative PSA. (Expert Opinion)
对于在根治性前列腺切除术中发现阳性淋巴结的患者,临床医生应根据病理学检查结果和术后PSA进行风险分层。(专家意见)
25. Clinicians may offer patients with positive lymph nodes identified at radical prostatectomy and an undetectable post-operative PSA adjuvant therapy or observation. (Conditional Recommendation; Evidence Level: Grade C)
对于在根治性前列腺切除术中发现阳性淋巴结且术后PSA无法检出的患者,临床医生可提供辅助治疗或观察。(有条件的推荐;证据水平:C级)
26. Clinicians should not routinely recommend adjuvant radiation therapy after radical prostatectomy. (Strong Recommendation; Evidence Level: Grade A)
临床医生不应常规推荐在根治性前列腺切除术后进行辅助放疗。(强烈推荐;证据水平:A级)
PRINCIPLES OF RADIATION
放疗的原则
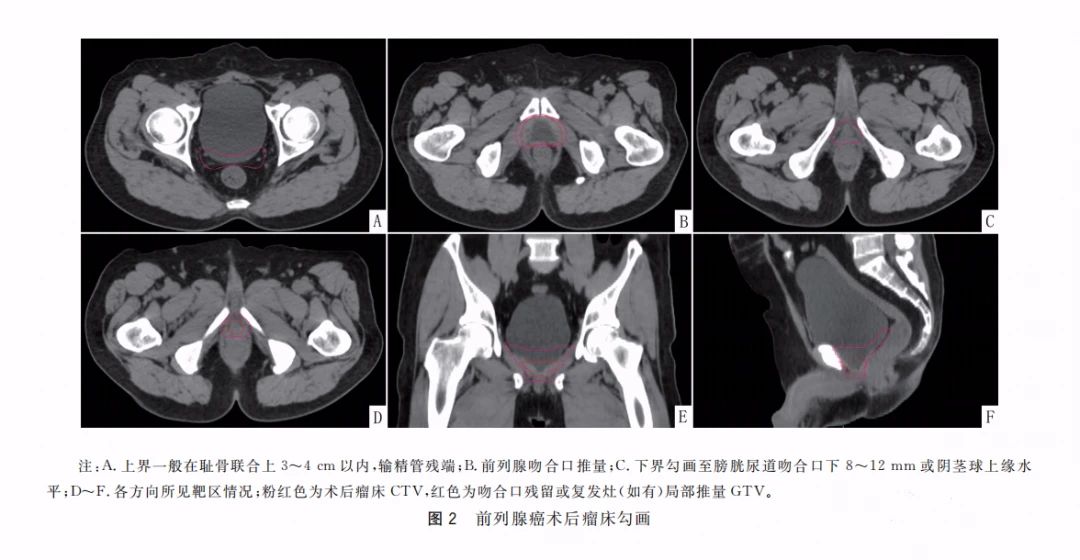
27. Clinicians should utilize available target localization, normal tissue avoidance, simulation, advanced treatment planning/delivery, and image-guidance procedures to optimize the therapeutic ratio of external beam radiation therapy (EBRT) delivered for prostate cancer. (Clinical Principle)
临床医生应利用可用的靶点定位、避开正常组织、模拟、先进的治疗计划/实施和图像引导技术,优化前列腺癌体外放射治疗(EBRT)的治疗比。(临床原则)
28. Clinicians should utilize dose escalation when EBRT is the primary treatment for patients with prostate cancer. (Strong Recommendation; Evidence Level: Grade A)
当EBRT是前列腺癌患者的初始治疗方案时,临床医生应进行剂量递增。(强烈推荐;证据水平:A级)
29. Clinicians may counsel patients with prostate cancer that proton therapy is a treatment option, but it has not been shown to be superior to other radiation modalities in terms of toxicity profile and cancer outcomes. (Conditional Recommendation; Evidence Level: Grade C)
临床医生可以告知前列腺癌患者,质子治疗是一种治疗选择,但在毒性情况和癌症结局方面,并没有证据表明质子治疗优于其他放疗方式。(有条件的推荐;证据水平:C级)
30. Clinicians should offer moderate hypofractionated EBRT for patients with low- or intermediate-risk prostate cancer who elect EBRT. (Strong Recommendation; Evidence Level: Grade A)
对于选择EBRT的低危或中危前列腺癌患者,临床医生应提供中度低分割EBRT。(强烈推荐;证据水平:A级)
31. Clinicians may offer ultra hypofractionated EBRT for patients with low- or intermediate risk prostate cancer who elect EBRT. (Conditional Recommendation; Evidence Level: Grade B)
对于选择EBRT的低危或中危前列腺癌患者,临床医生可以提供超低分割EBRT。(有条件的推荐;证据水平:B级)
32. In patients with low- or favorable intermediate-risk prostate cancer electing radiation therapy, clinicians should offer dose-escalated hypofractionated EBRT (moderate or ultra), permanent low-dose rate (LDR) seed implant, or temporary high-dose rate (HDR) prostate implant as equivalent forms of treatment. (Strong Recommendation; Evidence Level: Grade B)
对于选择放疗的低危或具有良好特征的中危前列腺癌患者,临床医生应将剂量递增的低分割EBRT(中度或超低)、低剂量率(LDR)永久性种子植入或高剂量率(HDR)临时前列腺植入作为同等的治疗形式为患者提供。(强烈推荐;证据水平:B级)
33. In patients with low- or intermediate-risk prostate cancer electing radiation therapy, clinicians should not electively radiate pelvic lymph nodes. (Strong Recommendation; Evidence Level: Grade B)
对于选择放疗的低危或中危前列腺癌患者,临床医生不应常规进行选择性盆腔淋巴结放疗。(强烈推荐;证据水平:B级)
34. In patients with low- or favorable intermediate-risk prostate cancer electing radiation therapy, clinicians should not routinely use ADT. (Moderate Recommendation; Evidence Level: Grade B)
对于选择放疗的低危或具有良好特征的中危前列腺癌患者,临床医生不应常规使用ADT。(中等推荐;证据水平:B级)
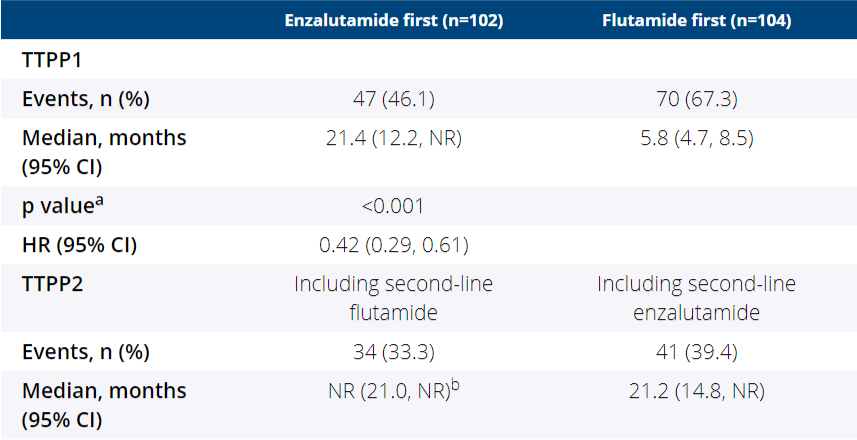
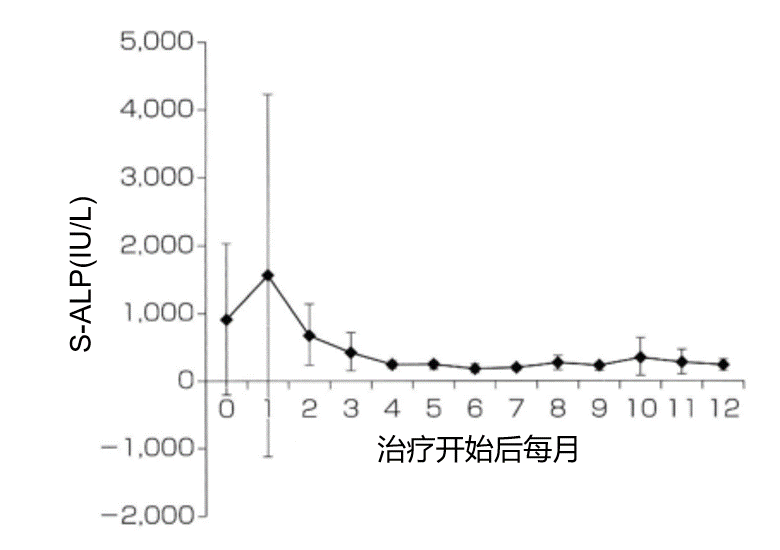
35. In patients with unfavorable intermediate-risk prostate cancer electing radiation therapy, clinicians should offer the addition of short-course (four to six months) ADT with radiation therapy. (Strong Recommendation; Evidence Level: Grade A)
对于选择放疗且具有不良特征的中危前列腺癌患者,临床医生应在放疗的同时提供短期(4-6个月)ADT。(强烈推荐;证据水平:A级)
36. Clinicians should offer moderate hypofractionated EBRT for patients with high-risk prostate cancer who are candidates for EBRT. (Moderate Recommendation; Evidence Level: Grade C)
对于适合EBRT的高危前列腺癌患者,临床医生应提供中度低分割EBRT。(中等推荐;证据水平:C级)
37. In patients with unfavorable intermediate- or high-risk prostate cancer electing radiation therapy, clinicians should offer dose-escalated hypofractionated EBRT or combined EBRT + brachytherapy (LDR, HDR) along with a risk-appropriate course of ADT. (Strong Recommendation; Evidence Level: Grade A/B)
对于高危或具有不良特征的中危前列腺癌患者,如果患者选择放疗,临床医生应提供剂量递增的低分割EBRT或EBRT+近距离放疗(LDR,HDR),同时根据患者风险提供适当的ADT疗程。(强烈推荐;证据水平:A/B级)
38. In patients with high-risk prostate cancer electing radiation therapy, clinicians may offer radiation to the pelvic lymph nodes. (Conditional Recommendation; Evidence Level: Grade B)
对于选择放疗的高危前列腺癌患者,临床医生可提供盆腔淋巴结放疗。(有条件的推荐;证据水平:B级)
39. When treating the pelvic lymph nodes with radiation, clinicians should utilize intensity-modulated radiation therapy (IMRT) with doses between 45 Gy to 52 Gy. (Strong Recommendation; Evidence Level: Grade B)
当对盆腔淋巴结进行放疗时,临床医生应进行调强放疗(IMRT),剂量为45 Gy-52 Gy。(强烈推荐;证据水平:B级)
40. In patients with high-risk prostate cancer electing radiation therapy, clinicians should recommend the addition of long-course (18 to 36 months) ADT with radiation therapy. (Strong Recommendation; Evidence Level: Grade A)
对于选择放疗的高危前列腺癌患者,临床医生应建议在放疗的同时进行长期(18-36个月)ADT。(强烈推荐;证据水平:A级)
41. When combined ADT and radiation are used, ADT may be initiated neoadjuvantly, concurrently, or adjuvantly. (Conditional Recommendation; Evidence Level: Grade C)
当ADT与放疗联合使用时,ADT可作为新辅助治疗、同期治疗或辅助治疗进行。(有条件的推荐;证据水平:C级)
42. When combining ADT with radiation therapy, clinicians may use combined androgen suppression (luteinizing hormone-releasing hormone [LHRH] agonist with an antiandrogen), an LHRH agonist alone, or an LHRH antagonist alone. (Expert Opinion)
当ADT与放疗联合使用时,临床医生可以使用雄激素抑制剂联合治疗(促黄体生成激素释放激素[LHRH]激动剂联合抗雄激素药)、单独使用LHRH激动剂,或单独使用LHRH拮抗剂。(专家意见)
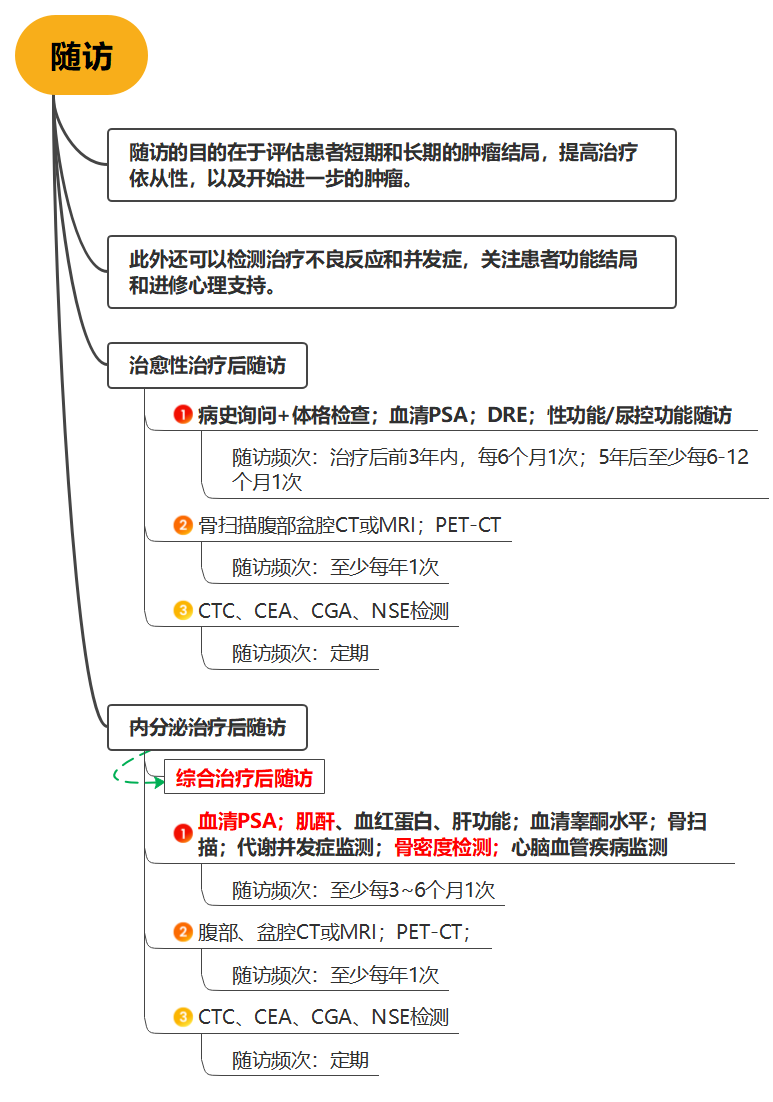
Follow-up after Treatment
治疗后随访
43. Clinicians should monitor patients with prostate cancer post therapy with PSA and symptom assessment. (Clinical Principle)
临床医生应通过PSA和症状评估对治疗后的前列腺癌患者进行监测。(临床原则)
44. Clinicians should support patients with prostate cancer through continued symptom management and encouraging engagement with professional or community-based resources. (Clinical Principle)
临床医生应通过持续的症状管理以及鼓励专业或社区资源参与,来支持前列腺癌患者。(临床原则)